Health
7 Things to Know About the Future of Healthcare Post-Pandemic

Global healthcare systems have undergone irreversible change due to the COVID-19 outbreak. We transition into the post-pandemic era. There will be several major developments that will influence the future of healthcare. This article will examine seven noteworthy innovations. Innovations that will reshape healthcare in the years ahead.
These developments deal with the quick uptake of telemedicine. It covers the increased attention on public health infrastructure. And it shows a paradigm shift in the way we approach and provide healthcare. This will have a tremendous effect on patient care and medical research. It will influence the general health and well-being of communities around the world. It will become clear as we examine them in more detail.

The Rise of Telemedicine
The COVID-19 epidemic has led to an exponential increase in the use of telemedicine. Especially between 2019 and 2020, the number of virtual medical consultations increased 46 times. Telehealth was gaining popularity before the epidemic, although it encountered difficulties with deployment and reimbursement.
During COVID-19, laws and reimbursement guidelines were shortly relaxed. This allowed telemedicine to gain widespread popularity in healthcare systems. To maintain its benefits, addressing regulations and ensuring fairness is vital.
With the rapid growth of Medical CPT codes like 99453, 99454, and 99457 used for remote monitoring services, this indicates the rise of preventive digital health solutions. CPT code lookup tools now make it easier for both patients and providers to identify and utilize relevant virtual care codes.
Patients can get help from telehealth in many ways, including increased accessibility. It’s also known for its ease of use and can lead to reduced expenses. Furthermore, telehealth offers the capacity for patients to get high-quality care from the comfort of their own homes. It provides for more effective workflows, enables the ability to scale up care delivery, and allows for remote monitoring of chronic illnesses for physicians. Research indicates that patients of all demographics are very satisfied with telemedicine services.
But we now enter the post-pandemic age, and a few significant telemedicine-related issues still exist:
- Payment Uncertainty: The COVID-19-introduced temporary waivers for telehealth coverage may expire, which could affect revenue. For widespread use, more precise reimbursement guidelines are essential.
- Technology Gaps: In many areas, the infrastructure for telehealth is still underdeveloped due to a lack of broadband access and integration capabilities with electronic health records. Providers must make investments in telemedicine technologies that are easy to use and interoperable.
- Obstacles to the User Experience: Poor virtual doctor-patient interactions can be problematic, and the absence of physical examinations is another concern. Additionally, technical issues can also have a detrimental effect on telehealth encounters. We must apply design thinking to improve engagement.
- Difficulties with Care Coordination: Inadequate coordination may result in disjointed care between virtual and in-person services. Organizations must improve telehealth integration with broader care systems.
Healthcare organizations should focus on continuous improvement of their telemedicine capabilities, including the implementation of coordinated care models and bidirectional data flows. They must ensure the presence of skilled clinicians.
These steps, combined with the use of CPT code lookup tools to streamline remote monitoring services and billing processes, can enhance the quality and effectiveness of telehealth services, leading to better patient care in the evolving landscape of healthcare. The post-pandemic era adopts blended models, with one that combines in-person and virtual treatment likely to become the standard.

Healthcare Infrastructure and Preparedness
COVID-19 revealed flaws in the global healthcare system. Going forward, it will be imperative to make investments in surge capacity. And also consider supply chain resilience, and disaster preparedness. We need a strong system for exchanging data between the public and business sectors. This can improve readiness for pandemics. Governments must also address the socioeconomic determinants of health. They must increase access to healthcare, and lower costs. To withstand future outbreaks, healthcare systems must be egalitarian and resilient.
Shift Towards Preventive Care
The pandemic highlighted the value of preventive care. This was because postponed treatments had a negative impact on health. Wellness-promoting lifestyle adjustments, early screening, and immunizations will become more common. Including remote patient monitoring. For example, there have already been new vaccine campaigns. There are also cancer screening programs, and chronic illness management initiatives launched. Population health and prevention must also be top priority in healthcare systems.
There is a renewed emphasis on preventive care. It is also driving the adoption of remote patient monitoring technologies. These allow providers to track key health metrics like blood pressure, heart rate, etc. It enables early interventions when needed.
Mental Health Takes Center Stage
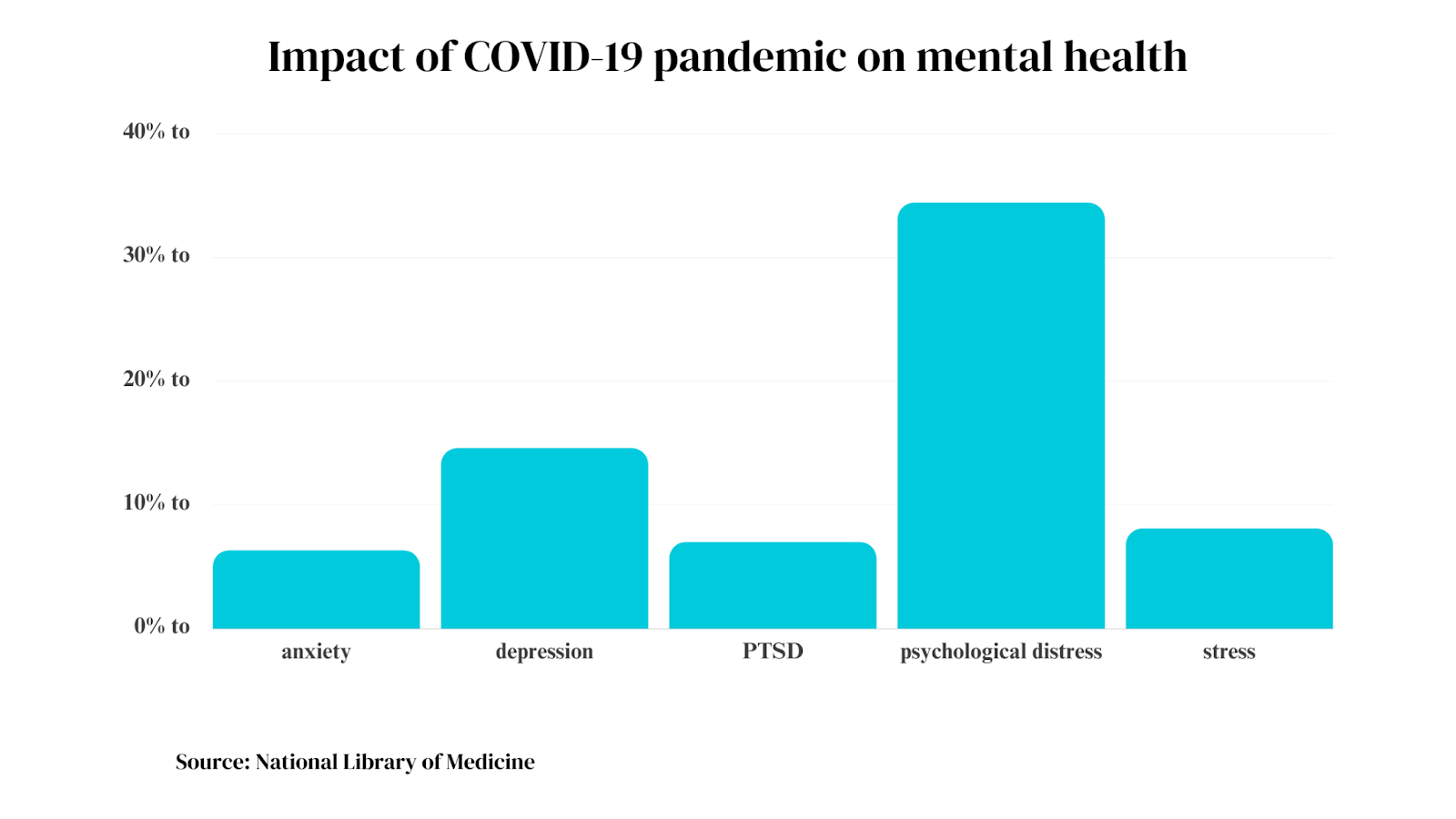
The pandemic’s effects on mental health have been profound. It has aggravated pre-existing issues and ignited brand-new ones. Frontline workers are struggling with depression, anxiety, PTSD, and fatigue. In all populations, social isolation has led to a rise in drug misuse and suicide thoughts. It has also increased domestic violence.
But even before COVID, mental healthcare facilities were beset by a lack of workers. They also struggled with insufficient funding. Although about 60% of Americans do not get treatment, and 1 in 5 suffer from mental illness. Shame is still a major obstacle. Since the epidemic has overwhelmed current services, there must be immediate action.
Going forward, healthcare policies must focus on mental wellbeing alongside physical health. Some strategies include:
- Integrating mental health services into primary and community care settings
- Promoting early screening, especially in high-risk groups
- Expanding access to mental healthcare through telemedicine and community partnerships
- Reducing stigma by raising awareness and promoting wellness conversations
- Increasing mental health funding, workforce training, and supportive housing initiatives
- Enabling employee wellness programs focused on building resilience
Addressing the pandemic’s mental health fallout requires a whole-of-society approach. An approach combining healthcare, government, nonprofit, and business efforts. Imagine a comprehensive public health strategy. One that integrates mental health promotion across social and institutional realms. This will be instrumental in managing this parallel pandemic.
Decentralization of Healthcare Services
Overburdened hospitals highlighted the need to diversify care settings. Ambulatory, home-based, and community care models will rise, improving access and outcomes. For instance, policy changes now enable more services to shift to retail clinics. They also shift to urgent care centers, and telemedicine. Decentralized care specialized services, alongside robust primary care networks, will define the future.
Innovations in Medical Technology
COVID-19 spurred healthcare innovation, accelerating telemedicine, vaccine development, and data analytics. Investments in emerging technologies like AI, IoMT, and robotics will continue growing. Precision medicine and genomic sequencing will enable personalized diagnoses and treatments. Regulations and interoperability frameworks must evolve in tandem to maximize these technologies’ impact.
Healthcare Policy and Universal Access
The pandemic showcased healthcare’s critical role as a public good. But it requires coordinated policy responses. It reinvigorated debates around universal healthcare. Policymakers must address coverage gaps, service access, and social barriers to seeking care. Comprehensive primary care and fair financing models are important. These including strong public health systems will be instrumental to democratizing healthcare access.
FAQs on the Future of Healthcare Post-Pandemic
How will the role of healthcare professionals evolve in the post-pandemic era?
Healthcare professionals will likely take on more diverse roles. They will emphasize preventive care and community outreach. There will be more focus on mental health support. All these concerns will add to their traditional responsibilities.
Will telemedicine replace in-person consultations?
Telemedicine will play a significant role. But in-person consultations will remain crucial for certain treatments, procedures, and patient populations.
How will the global healthcare community ensure better preparedness for future pandemics?
Enhanced global collaboration and investment in research will emerge. And robust healthcare infrastructures are some measures to prevent future healthcare crises.
Conclusion
In conclusion, the COVID-19 pandemic has been an inflection point for global healthcare. It has prompted unprecedented changes and challenges. We now move into the post-pandemic era. It is crucial to emphasize the importance of international collaboration and data sharing.
The pandemic has shown us that health crises transcend borders. A collective response is vital to safeguarding global health. By continuing to work together we can share knowledge and navigate the current challenges. It can also prepare us for future health threats.
The lessons learned from this pandemic underscore the need for solidarity and cooperation. We need a resilient and patient-centric healthcare system. One that can withstand the uncertainties of tomorrow.

Health
New Study Reveals Drinking Soda Pop Increases the Risk of Stroke

A recent report from global research indicates that excessive consumption of coffee or soda pop is associated with an increased risk of stroke, although the intake of black and green tea is correlated with a reduced risk. Excessive consumption of soda pop or coffee warrants caution!
Recent research indicates that it may substantially elevate the risk of stroke.
Consuming four cups of coffee daily elevates the risk of stroke, according to studies, although ingesting 3-4 cups of black or green tea daily typically offers protection against stroke. Additionally, consume more coffee; it may reduce your risk of mortality.
Recent findings from global research studies co-led by the University of Galway and McMaster University, alongside an international consortium of stroke researchers, indicate that soda, encompassing both sugar-sweetened and artificially sweetened variants such as diet or zero sugar, is associated with a 22 percent heightened risk of stroke. The risk escalated significantly with the consumption of two or more of these beverages daily.
Stroke Risk Fizzy Drinks and Soda Pop
The correlation between fizzy drinks consumption and stroke risk was most pronounced in Europe, the Middle East, Africa, and South America. Women exhibit the most elevated risk of stroke from bleeding (intracranial hemorrhage) associated with fruit juice beverages. Consuming over 7 cups of water daily diminishes the likelihood of stroke due to a clot.
Researchers observed that numerous items advertised as fruit juice are derived from concentrates and have added sugars and preservatives, potentially negating the advantages often associated with fresh fruit and instead elevating stroke risk.
Fruit juice beverages were associated with a 37 percent heightened risk of stroke resulting from bleeding (intracranial hemorrhage). Consuming two of these beverages daily increases the risk thrice.
Consuming over four cups of coffee daily elevates the risk of stroke by 37 percent, although lower consumption levels do not correlate with stroke risk. Conversely, tea consumption was associated with an 18-20 percent reduction in stroke risk. Additionally, consuming 3-4 cups daily of black tea, such as Breakfast and Earl Grey varieties, excluding green and herbal teas, was associated with a 29 percent reduced risk of stroke.
Consuming 3-4 cups of green tea daily was associated with a 27 percent reduction in stroke risk. Notably, the addition of milk may diminish or inhibit the advantageous effects of antioxidants present in tea. The lower risk of stroke associated with tea consumption was negated for individuals who added milk.
Disclaimer: This article is intended solely for informational reasons and should not be considered a replacement for professional medical counsel. Consistently consult your physician regarding any inquiries pertaining to a medical problem.
Related News:
Starbucks Faces Sales Decline Amid Price Fatigue and Rising Competition
Starbucks Faces Sales Decline Amid Price Fatigue and Rising Competition
Health
A Comprehensive Guide to Under Eye Creams

The delicate under eye area is often the first to show signs of aging, fatigue, and sun damage. Dark circles, puffiness, fine lines, and wrinkles can leave you looking tired and worn out, even after a good night’s sleep. This is where under eye creams come in. These targeted skincare products aim to address these concerns, offering a glimmer of hope for achieving a brighter, more youthful appearance. But with a plethora of under eye creams on the market, navigating the world of these products can feel overwhelming. In this blog, we will understand under eye creams, explore their benefits, and help you find the perfect solution for your unique needs.
The Undereye Area: Why Does It Need Special Care?
The skin under the eyes is significantly thinner and more delicate than the skin on the rest of your face. It also contains fewer oil glands, making it more prone to dryness and dehydration. These factors contribute to the specific concerns that tend to manifest in this area.
Take a look at the reasons why you need to opt for the best under eye cream –
- Dark Circles: These can be caused by various factors, including hyperpigmentation, genetics, sun damage, fatigue, and allergies. They appear as bluish, brownish, or purplish shadows under the eyes.
- Puffiness: Fluid retention, allergies, lack of sleep, and even consuming too much sodium can lead to puffiness, making the undereye area appear swollen.
- Fine Lines and Wrinkles: As we age, our skin naturally loses collagen and elastin, leading to the formation of fine lines and wrinkles. The delicate undereye area is particularly susceptible to these signs of aging.
However, it is also important to understand that only using the best under eye cream won’t help. You also have to make changes to your lifestyle for effective results.
Firstly, you need to ensure that you get adequate rest at night. Staying awake till late is not good for these delicate areas. Secondly, you need to drink plenty of water throughout the day. It will keep the skin hydrated and plump. Thirdly, you need to choose a well-balanced diet rich in fruits, vegetables, and whole grains and follow it religiously.

The Power of Under Eye Creams: Discover the Benefits
While under eye creams for Dark circles are not magical skincare products, they offer several potential benefits that can improve the overall appearance of your under eye area. These are –
- Hydration: The skin under your eyes is thinner and lacks the oil glands present elsewhere on your face. This makes it prone to dryness and dehydration, leading to a dull, tired appearance. Under Eye creams help plump and smooth the delicate under eye area, making you look refreshed and awake.
- Dark Circles: Dark circles can be caused by various factors, making your eyes look shadowed and tired. Under Eye creams with brightening properties can help address this concern.
- Depuffing: Fluid retention, allergies, or simply a long day can cause puffiness under the eyes. Under Eye creams can help reduce puffiness by promoting better circulation and decongesting the undereye area, leaving you looking refreshed and revitalized.
Choosing the Right Under Eye Cream: Finding Your Perfect Match
With a vast array of under eye creams available, selecting the right one requires considering your specific concerns and skin type. Here are some tips to keep in mind –
- For Dark Circles: Look for creams with vitamin C, kojic acid, or retinol to address hyperpigmentation.
- For Dry Skin: Look for creams formulated with hyaluronic acid, ceramides, or shea butter for intense hydration.
- For Sensitive Skin: Choose fragrance-free, hypoallergenic formulas to minimize irritation.

Application Tips for Optimal Results
Simply purchasing the under-eye cream is not enough. Here are some tips for maximizing the effectiveness of your under-eye cream –
- Apply on Clean Skin: Cleanse and pat dry your under-eye area before applying the cream. This ensures better absorption.
- Use a Pea-Sized Amount: Less is more! A pea-sized amount of cream is sufficient for both eyes.
- Gently Dab: Use your ring finger to gently dab the cream into the undereye area. Avoid dragging or rubbing, as this can irritate the delicate skin.
- Focus on the Bony Area: Apply the cream to the orbital bone, starting from the inner corner of your eye and moving outwards towards your temples.
- Let it Absorb: Allow the under-eye cream to fully absorb before applying any makeup.
- Consistency is Key: For optimal results, use your under-eye cream twice daily, once in the morning and again at night.

The best under eye cream for your dark circles
Lotus Organics+ Precious Brightening Under Eye Crème is one of the best under eye creams on the market. Enriched with 100% certified organic white peony extract, this lightweight under eye cream targets the delicate under eye area, addressing concerns like dark circles, puffiness, and fatigue.
For a revitalized and radiant look, incorporate the Lotus Organics+ Precious Brightening Under Eye Crème into your daily skincare routine!
SEE ALSO: FDA Approves New Non-Stimulant ADHD Medication “Onyda XR”
Health
Mind And Muscle: Exploring The Mental Benefits Of Regular Exercise

Feeling stressed or down lately? You’re not alone. Did you know that moving your body can boost your mood? This article will show you the powerful link between regular physical exercise and better mental health.
Get ready to feel inspired!
Key Takeaways
- Exercise helps your mind by making happy chemicals in your brain and makes you feel less stressed and more joyous.
- Doing activities like running or swimming changes your brain so you can think clearer and remember better. It also helps with sleep, making you rest well at night.
- Physical activity is good for people with depression, anxiety, ADHD, and other mental health issues because it improves mood and thinking skills.
- To get these benefits, start small like walking during breaks or doing simple exercises while watching TV. Also eat healthy foods to help your mind stay sharp.
- If starting an exercise routine seems hard, find fun activities you like doing, set clear goals, and maybe get a friend to join you for support.
How Exercise Impacts Mental Health
Regular exercise can affect mental health positively by releasing neurotransmitters and promoting neuroplasticity. It also increases the brain’s oxygen supply, leading to improved cognitive function and mood stabilization.
Releases neurotransmitters
Exercising makes your body release happy chemicals. Think of them like little messengers in your brain that help you feel good. One kind is called endorphins, and they play a big part in making you feel less pain and more joy—kind of like nature’s own happiness boost.
Another important one is serotonin, which helps keep your mood balanced and can make you feel calmer and happier.
I’ve felt this myself after a long run or a brisk walk—it’s like hitting a reset button on my stress levels. It doesn’t just happen by chance; it’s all thanks to these chemicals.
Doctors say this natural chemical release from physical activity can even work as well as some medicines for treating mental health issues.
Promotes neuroplasticity
So, after exercise lets out happy chemicals in the brain, it also works magic on neuroplasticity. This fancy word means your brain can change and adapt. Think of your brain as play-dough.
Exercising shapes this play-dough to help you learn and remember better. It fires up the creation of new connections between brain cells. Activities like jogging or swimming turbo-charge this process.
This is a big deal for mental health conditions like depression or anxiety disorder. Regular physical activity makes the hippocampus – that’s a part of the brain that helps with memory and learning – stronger and healthier.
A fit hippocampus means a sharper mind and better mood stability for people dealing with these tough challenges.
Increases oxygen supply to the brain
Moving from how exercise changes brain structure, it also boosts the flow of oxygen to your brain. This is like watering a plant; it helps your brain thrive and grow. More oxygen means your brain works better.
You think clearer and remember things easier.
I found this out myself after starting morning jogs. Before, my mind often felt foggy, especially mid-afternoon. But after making jogging a habit, that fog lifted. Science backs this up too—exercise gets more blood pumping through your heart to every part of your body, including the most critical part: your brain.
It’s about keeping your mental wellness in top shape too.
As Workout Guru https://workoutguru.fit/, we provide an extensive selection of workout exercises, routines, and valuable nutritional advice tailored to help our customers meet various fitness objectives. Whether it’s weight loss, muscle building, or improving overall health, our expert guidance and rich resources will set you on the right.
Mental Health Benefits of Regular Exercise
Regular exercise has numerous mental health benefits. It can help in relieving stress, boosting self-confidence, improving mood, enhancing sleep quality, and sharpening memory and thinking.
Additionally, it can also be beneficial for individuals dealing with depression, ADHD, anxiety, bipolar disorder, OCD,.
and PTSD.
Stress relief
Regular exercise is a powerful tool for reducing stress. Physical activity helps to lower the body’s stress hormones, such as cortisol. It also stimulates the production of endorphins, which are natural mood lifters in our brain.
These chemical changes in the brain can lead to reduced feelings of anxiety and better ability to handle everyday stresses.
Moreover, exercise offers an opportunity for distraction from day-to-day worries and allows people to find some quiet time to break out of the cycle of negative thoughts that can feed anxiety and depression.
In my own experience, I have found that just a few minutes of physical activity has an immediate effect on my overall mental well-being by helping me clear my mind and feel more relaxed throughout the day.
Incorporating exercises such as brisk walking or fitness training into your routine can significantly contribute to improved mental health. By finding moments for physical activity each day, we equip ourselves with a reliable defense against stress.
Improved self-confidence
Improved self-confidence is a significant benefit of regular exercise. Engaging in physical activity can lead to feeling better about yourself and your abilities. When you notice improvements in your physical fitness, it often translates into greater self-assurance and belief in what you can accomplish.
This boost in confidence extends beyond the gym or sports field and seeps into other areas of life, such as work, relationships, and personal goals. Incorporating exercise into your routine not only enhances your physical health but also plays a crucial role in building a positive sense of self-worth.
Regular exercise can contribute to heightened self-esteem, making individuals feel more capable and empowered in various aspects of daily living. As one gains strength and stamina through fitness activities, there tends to be an accompanying mental fortitude that positively impacts how challenges are approached and conquered.
Furthermore, the discipline required for consistent workouts fosters a sense of achievement that bolsters confidence levels over time.
Mood improvement
Regular exercise does wonders for your mood. The release of endorphins during physical activity can leave you feeling happy and uplifted. Moreover, it reduces feelings of anxiety and depression, making you feel more relaxed and at ease.
With improved sleep quality, sharper memory, and reduced stress levels due to regular exercise, your overall mood is greatly enhanced.
One significant aspect of regular exercise is its positive impact on mental health conditions such as depression, ADHD, anxiety, bipolar disorder, OCD, and PTSD. It’s like a natural remedy that actively works towards improving your emotional well-being whilst enhancing your physical health too.
So let’s now explore the ways we can incorporate exercise into our daily routines for optimal mental benefits in the next section.
Better sleep
Transitioning from mood improvement to better sleep, it’s evident that regular exercise plays a significant role in promoting better sleeping patterns. Engaging in physical activity helps regulate the sleep-wake cycle by increasing body temperature, which subsequently leads to deeper and more restorative sleep.
This is due to the release of endorphins during exercise, which not only reduce stress but also promote relaxation and enhance overall sleep quality. Individuals who incorporate moderate-intensity exercises into their routine tend to experience an improvement in both falling asleep and staying asleep, ultimately contributing to a more rejuvenating night’s rest.
Entities: Regular Exercise, Physical Activity, Endorphins
Tools: Sleep Tracker
Sharper memory and thinking
Exercise doesn’t just boost muscles, it also jazzes up your brain. Regular physical activity has been shown to enhance memory and thinking abilities. The increased blood flow and oxygen supply to the brain that comes with exercise can help improve cognitive function.
Studies have even suggested that physical activity could potentially reduce the risk of developing dementia or Alzheimer’s disease in later life.
One study found that as little as 120 minutes of moderate exercise per week could lead to improved cognitive function over six months. This means that a bit of regular exercise might just be the boost your brain needs when it comes to keeping sharp and focused!
Can help with depression, ADHD, anxiety, bipolar disorder, OCD, and PTSD
Exercise offers various mental health benefits and can assist in managing several conditions such as depression, ADHD, anxiety, bipolar disorder, OCD, and PTSD. Here’s how it helps:
- Depression: Exercise can alleviate symptoms of depression by increasing endorphins and reducing immune system chemicals.
- ADHD: Physical activity promotes focus and attention while reducing symptoms of hyperactivity and impulsivity.
- Anxiety: Regular exercise helps reduce anxiety levels by releasing tension and stress stored in the body.
- Bipolar Disorder: Exercise can help stabilize mood swings and reduce the severity of depressive and manic episodes.
- OCD: Engaging in physical activity aids in managing obsessive thoughts and compulsive behaviors.
- PTSD: Exercise assists in reducing the intensity of flashbacks and intrusive thoughts associated with trauma.
By incorporating regular exercise into your routine, you’ll be taking a proactive step toward improving mental well-being for these specific conditions as well as overall holistic health.
Tips for Incorporating Exercise into Your Routine
Incorporating exercise into your routine can be done by making small changes such as taking the stairs instead of the elevator, walking during your lunch break, or doing simple exercises while watching TV.
Together with a balanced diet, even these little efforts can make a big difference in improving mental and physical well-being. If you’d like to learn more about how to easily fuse physical activity into your daily life for maximum impact on your mind and body, keep reading!
Diet’s impact on mental health
A balanced diet is not just crucial for physical health but also plays a significant role in mental well-being. Certain nutrients, like omega-3 fatty acids found in fish, and antioxidants present in fruits and vegetables, can positively impact mood and cognitive function.
Likewise, consuming excessive amounts of processed foods high in sugar and unhealthy fats may contribute to an increased risk of developing mental health disorders such as depression and anxiety.
It’s essential to maintain a healthy diet that includes a variety of nutrient-rich foods to support overall mental wellness.
Integrating whole grains, lean proteins, healthy fats, and ample fruits and vegetables into daily meals can provide essential vitamins and minerals which are vital for brain function.
These nutrients aid in neurotransmitter synthesis – the chemical messengers responsible for regulating mood. Additionally, staying hydrated with water or herbal teas can help prevent mood swings caused by dehydration.
My personal experience has shown me the substantial impact of adopting a balanced diet on my own mental state – feeling more energized while maintaining a stable mood throughout the day.
Starting an exercise routine
Here’s the content for “Starting an exercise routine” in a well-structured, casual tone:
Ready to kickstart your exercise routine? Let’s make it happen.
- Set realistic goals: Ensure your exercise plan aligns with your abilities and time constraints; take small steps towards larger objectives.
- Mix it up: Keep things interesting by combining various activities such as walking, swimming, and cycling.
- Schedule sessions: Incorporate exercising into your daily schedule, treating it like any other important appointment.
- Find a workout buddy: Team up with a friend or family member for mutual motivation and support.
- Celebrate milestones: Acknowledge and reward progress to stay encouraged and committed.
Now that we have the tools in hand, let’s understand how diet impacts mental health.
Overcoming obstacles
Starting an exercise routine can be challenging, but overcoming obstacles is essential for long-term success. Here are some strategies and tips to help you overcome barriers in your path to regular exercise:
- Set realistic goals: Start with achievable targets that fit into your daily life, and gradually increase the intensity and duration as you progress.
- Find activities you enjoy: Experiment with different types of exercise until you find something that brings you joy, whether it’s dancing, hiking, or playing sports.
- Create a support system: Surround yourself with people who encourage and motivate you to stay active, such as workout buddies or joining group fitness classes.
- Manage time effectively: Schedule your workouts just like any other important appointment, and prioritize physical activity as an integral part of your routine.
- Adapt to setbacks: Understand that slips and relapses are normal; instead of being discouraged by them, learn from setbacks and recommit to your exercise plan.
- Address mental barriers: Recognize and challenge negative thoughts about exercising, and practice positive self-talk to build a resilient mindset.
- Seek professional help if needed: If you’re struggling with persistent obstacles or motivational issues, consider consulting a fitness trainer or a mental health professional for guidance.
By incorporating these strategies into your journey of regular physical activity, you can steadily overcome the barriers preventing you from reaping the mental health benefits of exercise.
Finding motivation and support
Regular exercise can be challenging – overcoming obstacles is part of the journey. Here are some tips for finding motivation and support:
- Surround yourself with like-minded individuals who can inspire and encourage you. Having a supportive community can make a significant difference in staying motivated.
- Set achievable short-term goals and celebrate your progress. Small victories can keep you motivated on a daily basis, ultimately leading to long-term success.
- Consider working with a personal trainer or joining group fitness classes to stay engaged and accountable.
- Use technology to your advantage – there are countless apps and online communities designed to support and motivate individuals in their fitness journeys.
- Keep a journal to track your progress and reflect on how far you’ve come, helping to reinforce positive habits.
Staying motivated and finding support throughout your exercise routine can significantly impact both your physical and mental well-being, helping you achieve long-term success in maintaining an active lifestyle.
Conclusion.
Exercise isn’t just for your body; it’s a game-changer for the mind too. It triggers feel-good chemicals, boosts brainpower, and fights off stress and anxiety. Don’t forget: regular exercise is not only about getting fit but also about nourishing your mental health.
Workout Guru offers a free database of over 5000 exercises to match every conceivable fitness wish or need. If you truly desire to enhance and maintain your fitness levels, there’s no better place to start than here at Workout Guru.
So, lace up those sneakers and give your mind a mighty workout!
FAQs
1. How does exercise help your mind?
Exercise makes your body release chemicals like endocannabinoids and b-endorphins. These make you feel happy and less stressed. It’s like getting a natural high, often called a runner’s high, that boosts your mood.
2. Can working out help with mental illness?
Yes, it can! Physical activity is good for the brain and can be part of treating mental illnesses such as depression and anxiety. It works well alongside other treatments like cognitive behavioral therapy (CBT), meditation, and sometimes medications.
3. Does exercise do anything for stress?
Absolutely! When you exercise, your heart rate goes up in a good way which helps reduce stress levels. Plus, focusing on movement helps take your mind off worries.
4. What are some long-term benefits of regular physical activity on the brain?
Regular workouts can slow down signs of aging in the brain, keeping it sharp longer. They also help control weight which reduces risks related to obesity such as heart disease and type 2 diabetes.
5. Can exercise improve symptoms for people with schizophrenia or other serious mental conditions?
It sure can! Exercise has been shown to help manage negative symptoms of schizophrenia and improve overall quality of life for those dealing with psychotic disorders by reducing side effects from antipsychotic drugs.
6. How does being active affect sleep?
Getting enough physical activity during the day can lead to better sleep at night including more deep sleep cycles which are crucial for feeling rested.
Post Disclaimer
The above article is sponsored content any opinions expressed in this article are those of the author and not necessarily reflect the views of CTN News- Chiang Rai Times. For detailed information about sponsored content policy click here.
People Also Reading:
The Ultimate Guide to Knowledge Management: Exploring Intranets and Wikis
-

 News4 years ago
News4 years agoLet’s Know About Ultra High Net Worth Individual
-
Entertainment3 years ago
Mabelle Prior: The Voice of Hope, Resilience, and Diversity Inspiring Generations
-
News11 years ago
Enviromental Groups Tell Mekong Leaders Lao Dam Evaluation Process Flawed
-

 Health4 years ago
Health4 years agoHow Much Ivermectin Should You Take?
-

 Tech3 years ago
Tech3 years agoTop Forex Brokers of 2023: Reviews and Analysis for Successful Trading
-

 Lifestyles3 years ago
Lifestyles3 years agoAries Soulmate Signs
-

 Entertainment3 years ago
Entertainment3 years agoWhat Should I Do If Disney Plus Keeps Logging Me Out of TV?
-

 Health4 years ago
Health4 years agoCan I Buy Ivermectin Without A Prescription in the USA?